Receiving a diagnosis of Barrett’s esophagus can be unnerving. And the potential complications of this condition can be alarming. The good news is that a gastroenterologist can help you manage this condition and reduce your risk of esophageal cancer.
On this page, we’ll first explain what Barrett’s Esophagus is. Then we will discuss the causes and symptoms so that you know when to see a doctor. Lastly, we’ll explain the diagnosis and possible treatment recommendations.
What is Barrett’s Esophagus?
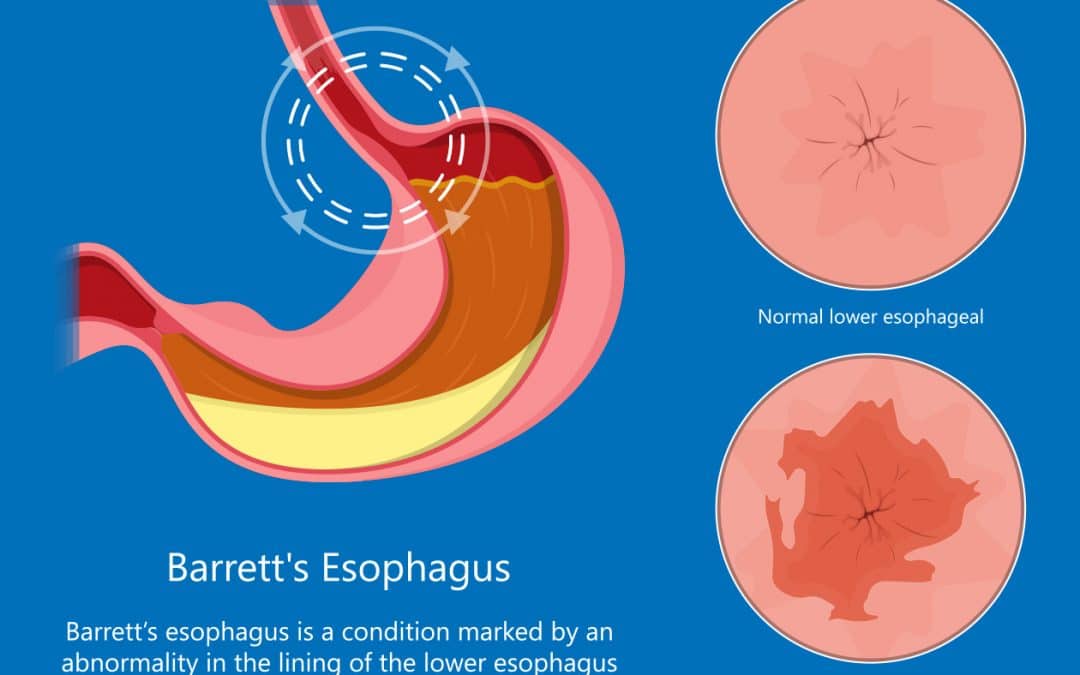
Barrett’s esophagus is a change in the tissue lining your esophagus. With this condition, the lining of the lower esophagus changes over time and starts to look like the small intestine instead of the esophagus.
A normal esophagus lining should have a pink and shiny color. The lining of the small intestines, and Barrett’s, looks red and velvety. The problem with this transformation in the lower esophagus is that Barrett’s is a precancerous condition, and if left untreated, it could transform into cancer. According to the NIH, men are twice as likely to develop Barrett’s esophagus as women.
Understanding Dysplasia
The National Cancer Institute defines dysplasia as a term used to describe the presence of abnormal cells within a tissue or organ. Dysplasia is not cancer, but it may sometimes become cancer.
Barrett’s Esophagus Without Dysplasia
Having Barrett’s esophagus WITHOUT dysplasia means you have intestinal cells being replaced by esophageal cells, but there are no signs of precancerous cells. With this diagnosis, you’ll need an upper endoscopy every two to three years to monitor your condition.
Barrett’s Esophagus With Dysplasia
Having Barrett’s esophagus WITH dysplasia occurs when there are precancerous changes in the cells of the esophagus. A diagnosis of Barrett’s esophagus with dysplasia increases your risk of esophageal cancer. But this doesn’t mean you will get cancer. With this diagnosis, more frequent monitoring is common to prevent cancer from developing.
Barrett’s esophagus has two grades of dysplasia: low-grade and high-grade.
- Low-Grade Dysplasia – This diagnosis means that you have some abnormal cells, but most are unaffected.
- High-Grade Dysplasia – This diagnosis indicates that cells in your esophagus have developed extensive abnormalities.
Symptoms and Causes of Barrett’s Esophagus
Causes
The exact cause of Barrett’s esophagus is unknown. However, it is most often detected in people with GERD. This chronic condition occurs when gastric juice, bile, or stomach acid goes up into the esophagus. If left untreated, this reflux can burn the lining of the esophagus and cause ulcers or esophagitis, which can transition to Barrett’s esophagus over time. But you can also have Barrett’s esophagus without having GERD.
- Please visit our GERD webpage to learn more about this digestive condition.
After the acid reflux damage occurs, the esophagus tries to heal itself. During this process, the cells can change to the type of cells found in Barrett’s esophagus.
Symptoms
Many people with Barrett’s esophagus don’t experience symptoms at all. However, the symptoms that patients may experience are due to GERD and can include the following:
- Frequent heartburn
- Trouble swallowing food
- Dry cough
- Hoarseness
- Vomiting blood
- Chest pains
- Sleep apnea
When should I see a Doctor for Reflux?
Current recommendations are that if you have acid reflux symptoms more than three times a week for more than 1-2 years, you should go in and be evaluated. The complications of acid reflux are preventable if caught early and treated. Also, the risk of progression of Barrett’s esophagus to esophageal cancer can be reduced if detected and treated early.
Diagnosing Barrett’s Esophagus
When patients present with the symptoms described in the previous Symptoms section, their doctor may want to screen them for Barrett’s esophagus. This evaluation would include an endoscopy, which allows your doctor to view the inside of your esophagus. During the upper endoscopy, your gastroenterologist will look for evidence of chronic acid reflux and the red or salmon-colored mucosa at the lower end of the esophagus that indicates Barrett’s may be present.
Typically, a couple of small pinch biopsies in this area are taken and sent to a pathologist to look for Barrett’s. The pathologist will also “stage” the Barrett’s to better indicate the cancer risk.
The first stage of Barrett’s is known as intestinal metaplasia. Over time this can progress through what’s known as low-grade dysplasia, then high-grade dysplasia, and then on to cancer. The goal is to catch it before it starts transforming into dysplasia.
How is Barrett’s Esophagus Treated?
Treatment options for Barrett’s esophagus are dictated by the level of dysplasia, which is determined by the biopsies taken during the endoscopy procedure. There are three levels of dysplasia… no dysplasia, low-grade dysplasia, and high-grade dysplasia.
No Dysplasia
If a diagnosis of Barrett’s esophagus is made, ideally, you would want no dysplasia. In this case, your doctor would typically recommend medications to help treat the acid exposure, and they would try to cut out other risk factors like tobacco and minimize alcohol. Also, you would follow up with endoscopy exams every 2-3 years, depending on risk factors, to monitor for any changes.
Low-Grade Dysplasia
A second pathologist evaluating the biopsies would always confirm a low-grade dysplasia diagnosis. This is done due to the complexity of diagnosing the level of dysplasia. If low-grade dysplasia is found, you would go on high-dose acid suppression and get endoscopic surveillance every six months until the dysplasia either goes away or continues to progress.
If the dysplasia continues progressing, then your doctor would consider ablation of the dysplasia. The Halo procedure is the most common and effective current method for Barrett’s ablation. What’s involved in this procedure is an upper endoscopy and then the passage of a small probe that destroys the dysplastic Barrett’s with radiofrequency ablation (heat energy).
This procedure is not done for Barrett’s without dysplasia because the procedure’s risks are higher than the risk of progression of non-dysplastic Barrett’s to dysplasia.
High-Grade Dysplasia
A diagnosis of high-grade dysplasia will also always have the same second pathology evaluation as previously mentioned with low-grade dysplasia. Also, radiofrequency ablation is a standard initial treatment for this level of dysplasia.
In addition, alternative therapies your doctor may recommend are cryotherapy (freezing of the abnormal cells) or photodynamic therapy (light-sensitive chemicals and lasers are used to kill the abnormal cells). If a specific focus of high-grade dysplasia is found, it can be removed endoscopically with endoscopic ultrasound and mucosal resection. The goal is to prevent high-grade dysplasia from becoming esophageal cancer.
Barrett’s Esophagus Prevention
Barrett’s esophagus is a life-long condition that can progress over time. You will need regular screening and treatment to decrease your risk of esophageal cancer.
Making lifestyle changes to reduce symptoms of GERD can also prevent your condition from worsening. The best way to keep the lining of your esophagus healthy is to address heartburn or GERD symptoms. People with ongoing, untreated heartburn are much more likely to develop Barrett’s esophagus.
Other ways to decrease your risk factors include:
- Avoid drinking alcohol and smoking, both of which can irritate esophageal tissue.
- Maintain a weight that’s healthy for you. Obesity makes you more susceptible to disease.
- Avoid trigger foods for acid reflux. Anything fatty, acidic, or highly caffeinated should be avoided.
If you have specific concerns about creating a diet to reduce the risk of aggravating the damaged tissue in your esophagus, ask your doctor to make a particular recommendation, or they may refer you to a dietician.
A Note from Dr. Havranek
Being diagnosed with Barrett’s esophagus isn’t a cause for alarm. But it is good information to have. Consider the diagnosis extra motivation to…
- Manage your GERD symptoms.
- Keep your regularly scheduled endoscopy tests.
These two things will ensure you do everything you can to stay well. If you want to discuss acid reflux symptoms or if you should be evaluated for Barrett’s esophagus, please call our office at (210) 615-8308 or schedule an appointment online.