Gas and bloating. If I could find a cure for this I would be on a beach right now somewhere sipping a Mai-Tai. Instead I’m here at my desk writing about gas and bloating. One of the most frustrating problems I help my patients with here in San Antonio, TX is gas and bloating. It’s something I battle myself at times. It can range from a grumbling sound to feeling like something is moving in your abdomen to belching and flatus and distention. It can be an occasional nuisance or a daily problem. My patients describe abdomens that cramp, bloat and at times get so big they feel pregnant. None of us like to be gassy and bloated (except maybe my brother) but most all of us experience it at one time or another. The most frustrating problems we deal with as physicians are those for which we don’t have great treatment, and this is one of those.
UPDATE: I’ve had a lot of success treating bloating in my practice with a natural product called Atrantil since posting this article. It was developed by a gastroenterologist in Dallas and targets the bacterial overgrowth in the small bowel that creates bloating symptoms for many. My recommendation is that if you bloat after eating certain foods that you look into Atrantil as a possible remedy to your bloating symptoms in addition to a low carbohydrate diet.
To understand how to best battle gas and bloating we need to first better understand what causes it. Most all gas and bloating we experience is the result of bacterial fermentation of food that we eat. There are many reasons these bacteria ferment our food. It may be due to our body’s inability to break down and or digest certain carbohydrates- lactose intolerance is an example of this. It may be due to an excess of enteric bacteria in our small bowel- small intestinal bacterial overgrowth (SIBO) is an example of this. Some people have a heightened sensitivity to physiologically normal amounts of gas and distention- irritable bowel syndrome (IBS) is an example of this. There are no great “anti-gas” medications that exist. We try things like antispasmodics, simethicone (breaks down gas bubbles), probiotics and digestive enzymes with moderate or limited success. Evidence is beginning to show more that the answer lies in what we eat. By changing our focus to our diet most of these symptoms can be reduced or eliminated. But the big question is what diet changes to make. That’s where FODMAPs come in.
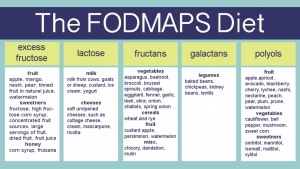
FODMAPs, or fermentable oligosaccharides, disaccharides, monosaccharides and polyols, seem to be the key. A nice study was recently published in one of the journals I regularly read, Gastroenterology, January 2014, showing that a diet low in FODMAPs reduces symptoms of IBS in people. Patients experienced less bloating, pain and passage of flatus while on a diet low in FODMAPs. They also had greater satisfaction with stool consistency. I won’t bore you with the details of the study, you can read the whole article by clicking on this link to the Gastroenterology Journal. Instead, let’s talk about the recommended diet changes. Remember that this is a guide. As you began to play with and focus on your individual diet you will find the foods that trigger your symptoms. The key is dedication and giving it a chance to work, diet changes are never easy.
FODMAPs are carbohydrates found in foods. Not all carbohydrates are FODMAPs. The main ones to focus on are fructose (fruits, high fructose corn syrup ); lactose (dairy products); fructans (wheat, onion, garlic); galactans (lentils, legumes); polyols (artificial sweeteners, mannitol, stone fruits like avocado, cherries, peaches). These are foods that are commonly not digested well and are fermented by our bacteria.
If you have tried the FODMAP diet or a variation to reduce bloating symptoms, please submit a comment and I would be happy to share your experience.
Written by: Russell Havranek, MD


Thank you for this article, Dr Havranek. I was wondering if you have had success treating ibs-c with antibiotics? I read Dr Pimentel’s book , IBS – A New Solution, in which he indicates that he has helped people with his Cedars-Sinai protocol. Thanks again!
Good question and yes I have. We do a lot of testing for small bowel bacterial overgrowth with hydrogen detecting breath test machines. Problem is, a percentage of the population has mainly methane producing bacterial that won’t show up on the breath tests. In my experience, those with IBS symptoms and diarrhea tend to have more hydrogen producing organisms and those with IBS with constipation symptoms tend to have more methane producing ones. I have never done the study but that is my experience. Having said that when I have a patient with IBS-C symptoms that are not responding to traditional treatments I always offer round of GI antibiotics and probiotics. I hope this helps. Good luck!
Dr Havranek,
Ive taken the IgG test for food allergies and recently got on a low fodmap diet along with some supplements that were suggested to me. I had severe pain that was debilitating at times. However since then there is still a dull nawing pain, along with chronic uritis. The pain is not nearly as intense. I have also been doing ileocical valve messages. I believe I have antibiotic caused SIBO however I have only taken the IgG test. Do you recommend getting the Hydrogen Breath tests along with a FODMAP diet?
We frequently see patients with these type of symptoms and the list of causes is a mile long. You are on the right track with what you have done so far but when the symptoms persist, as in your case, I would recommend a more comprehensive evaluation. This would include the hydrogen breath tests as well as diet changes like a FODMAP diet. Unfortunately, due to HIPAA regulations I cannot provide recommendations towards specific treatment regimens online. I invite you to schedule an appointment with my office or your gastroenterologist to allow for a complete evaluation. At that time, a full discussion regarding a hydrogen breath test could occur as well. Good luck.