A patient brought me an article last week from Reader’s Digest magazine that listed different questions you should ask your gastroenterologist prior to your colonoscopy. I felt that two of them were important to comment on that relate to the quality indicators for colonoscopy. In medicine, a lot of money and time is spent on what we call Quality Indicators – things that help us predict if our colleagues, or ourselves, are practicing the best medicine we can. That article prompted me to write this blog.
We track quality indicators closely in my group as we pride ourselves on being some of the best physicians in the San Antonio, TX area. Also, I serve on the physician review committee at Methodist Hospital here in San Antonio, TX to help make sure our colleagues are performing good medicine as well.
What should you ask your Gastroenterologist prior to Colonoscopy?
Withdrawal Time. The accepted minimum standard for withdrawal time in the USA and UK is 6 minutes. This is not the length of the entire exam but is the amount of time the gastroenterologist spends pulling the scope back out of the colon and looking around for colon polyps. Unfortunately, there are still too many gastroenterologists that are in a hurry, for many reasons, and don’t spend enough time actually looking for polyps. There are multiple papers demonstrating that physicians will find a larger number of significant polyps when they take at least 6 minutes or more on withdrawal time. And that’s why you’re there, to have your polyps found and removed. I did a recent review of my procedural data and found that I spend on average 13.4 minutes on withdrawal time, which more than twice the accepted minimum standard. It’s your health, quality matters!
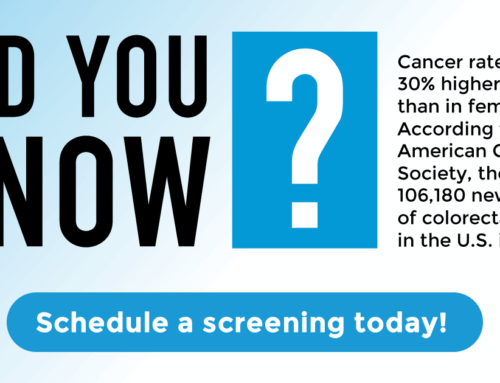
Adenoma Detection Rate. The second main indicator of quality is the amount of polyps your gastroenterologist finds on average. Adenomas, precancerous lesions arising throughout the colon, are the target of screening colonoscopies. Removing adenomatous polyps decreases the incidence of colorectal cancer, a leading causes of morbidity and mortality. Current guidelines suggest screening colonoscopy adenoma detection rates of 15% for women and 25% for men. This is the percent of female and male patients your gastroenterologist should find adenomatous polyps in during screening colonoscopy based on the incidence of adenomas in our population. Rates lower than this suggest they are not as thorough as they should be when looking for polyps, and are most likely missing polyps. The incidence of precancerous polyps is about that high in our population. I reviewed my polyp detection, and found I have an adenoma detection rate overall of 37.8% – which is well above the accepted standard for quality.
Hopefully this commentary shows that Quality Indicators matter when evaluating a gastroenterologist’s thoroughness in performing colonoscopy. All gastroenterologists in the San Antonio, TX area should be aware of their quality indicator procedural data and make it available to patients when requested, so don’t be hesitant to request that information prior to your colonoscopy. I review my quality indicator data quarterly to make sure that I continue to provide my patients great medical care.
I welcome any questions related to the quality indicators described in this commentary. Have a great day!