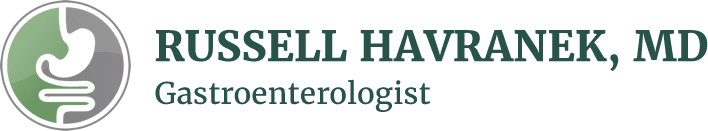
Esophageal cancer is the sixth leading cause of cancer-related deaths worldwide. Unfortunately, the incidence of some types of esophageal cancer is on the rise.
With this in mind, it’s important to be aware of certain factors that can put you at greater risk.
This article will discuss what esophageal cancer is and what causes it. We’ll also highlight how you can lower your likelihood of esophageal cancer.
What Is Esophageal Cancer?
Esophageal cancer is cancer that affects the esophagus — the muscular tube that connects the mouth and stomach. Esophageal cancer starts in the inner lining of the esophagus and can spread to the outer layers as it grows.
The two most common types of esophageal cancer are:
- Adenocarcinoma. This type of cancer occurs in glandular cells that produce mucus. Adenocarcinoma often starts near the stomach in the lower part of the esophagus. Alarmingly, this is the fastest-growing cancer in the United States. Cases of esophageal adenocarcinoma have significantly increased in the last 40 years. Adenocarcinoma makes up 80% of all esophageal cancer cases in the United States.
- Squamous cell carcinoma. This type of cancer affects squamous cells, which line the surface of the esophagus. Squamous cells are flat, thin cells that look like fish scales. Most cases of squamous cell carcinoma occur in the upper and middle parts of the esophagus. This type of cancer is the most common esophageal cancer worldwide. But squamous cell carcinoma cases in the United States have decreased in recent years.
Esophageal Cancer Symptoms
Generally, esophageal cancer doesn’t cause symptoms early on. Symptoms usually occur after the tumor in the esophagus grows larger.
Common esophageal cancer symptoms include:
- Difficulty swallowing (dysphagia)
- Unintentional weight loss
- Chest pain (pressure or burning)
- Worsening indigestion or heartburn
- Coughing or hoarseness
When to See a Gastroenterologist
If you experience any of the above esophageal cancer symptoms, you should see a gastroenterologist.
Having one or more symptoms doesn’t mean you have esophageal cancer. Many conditions can produce similar symptoms. But it’s important to be evaluated by a medical professional to find the cause and get treatment. Treatment often has the best outcome when started early.
Other signs to see a GI doctor include:
- Pain with swallowing. This may be a sign that you have reflux or an obstruction in the esophagus.
- Men with chronic acid reflux who frequently smoke or drink alcohol. Esophageal cancer is most common in men in the United States. This factor, combined with tobacco and alcohol consumption, increases the risk of esophageal cancer.
- A personal history of reflux. Chronic reflux can irritate the sensitive lining of the esophagus. Seeing a GI doctor can help you manage reflux and prevent potential complications like esophageal cancer.
- A family history of esophageal or gastric cancer. Some types of esophageal cancers have a hereditary component. If cancer runs in your family, frequent screening can catch it early or prevent it from starting in the first place.
- Dark blood in the stool. Blood in the stool that appears dark like tar is a sign of bleeding in the upper digestive tract, such as the esophagus. Bleeding in the esophagus can lead to anemia, a condition that makes you feel tired due to the lack of healthy red blood cells. Blood in the stool is never normal and is always a reason to see a doctor.
Common Causes of Esophageal Cancer
The exact cause of esophageal cancer is not known. But certain factors can increase your risk by damaging the DNA of cells that line the inside of the esophagus. Long-term damage to the esophagus increases the likelihood of esophageal cancer.
Common causes of esophageal cancer include:
- Smoking and tobacco use
- Alcohol consumption
- Achalasia
- Plummer-Vinson syndrome
- Swallowing lye
- GERD
In addition, people with Barrett’s esophagus are at a higher risk of esophageal cancer. Keep reading to learn more about this condition.
Barrett’s Esophagus
Barrett’s esophagus is a condition that results in damage to the lower part of the esophagus. This damage causes the cells in the esophagus to become more like intestinal cells.
Typically, the inside of the esophagus is pink and flat. But Barrett’s esophagus changes the lining of the esophagus to become red and thickened.
GERD is the most significant risk factor for Barrett’s esophagus. Repeated exposure of the esophagus to stomach acid, bile, and gastric juice can wear away at the lining of the esophagus. Barrett’s esophagus is more serious than heartburn because it involves long-term damage that results in cellular changes.
Most people with Barrett’s esophagus don’t develop esophageal cancer. But it’s essential to monitor this condition with your GI doctor to detect abnormal cellular changes as soon as possible.
Treatment options for Barrett’s esophagus may include:
- Medication
- Radiofrequency ablation
- Cryotherapy (freezing of the abnormal cells)
- Photodynamic therapy (light-sensitive chemical and laser can kill the abnormal cells)
- Endoscopic mucosal resection
- Surgery
How to Reduce Your Risk of Esophageal Cancer
You can reduce your risk of esophageal cancer by:
- Limiting or avoiding alcohol and tobacco. Alcohol and tobacco are both known carcinogens. Consuming either of these alone multiplies your risk of cancer, and combining the two is even worse. Limiting your alcohol intake to one to two servings instead of many can lower your risk of esophageal squamous cell carcinoma. If you smoke, you should try to cut out tobacco completely.
- Receiving treatment for reflux. Reflux that consistently occurs two or more times per week can damage your esophagus. Getting your reflux under control with medication or diet and lifestyle changes can prevent GERD from progressing to Barrett’s esophagus. Here are 10 ways to reduce symptoms of reflux.
- Maintaining a healthy weight. Obesity is linked to several different types of cancer. Visceral obesity, or increased belly fat, can increase your risk of esophageal adenocarcinoma. You can lower your risk by staying physically active.
- Eating a plant-based diet. Plant-based diets are rich in fiber, vitamins, and minerals. Incredibly, research shows that high fiber diets can decrease your risk of esophageal cancer. The more fiber you eat, the lower your risk of Barrett’s esophagus and esophageal cancer.
Diagnosing Esophageal Cancer
Diagnosing esophageal cancer starts with obtaining a medical history and performing a physical examination. Depending on the clinical findings, the doctor can perform additional testing.
Several tests can diagnose esophageal cancer. The most common tests are:
- Barium Swallow X-ray. This test involves drinking a chalky liquid called barium that coats the walls of the esophagus. You then undergo x-ray imaging, which outlines the barium in the esophagus. A barium swallow x-ray can detect cancer, but it can’t determine how far along it is.
- Upper endoscopy. During this test, the doctor passes an endoscope (a thin, flexible tube with a light and camera) down your throat while under sedation. This allows the doctor to see inside the esophagus. By inserting special instruments through the endoscope, the doctor can biopsy any abnormal tissues. Tissue samples are then sent to a lab to find out more information, such as the type of cancer.
Increasing Awareness
Sadly, esophageal cancer is often diagnosed in the later stages due to a lack of early symptoms. With the growing incidence of esophageal adenocarcinoma in the United States, it’s more important than ever to understand your risk factors.
The good news is that you can actively reduce your risk of esophageal cancer by making healthy diet and lifestyle choices. As always, you should never ignore digestive symptoms because severe conditions like cancer are much more treatable in their early stages.
You should see a GI doctor if you have:
- Persistent reflux
- A family history of esophageal or gastric cancer
- Difficulty swallowing
- Unintentional weight loss
- Chest pain
- Coughing or hoarseness
- Black, tar-like stools
If you’re located in the San Antonio area, you can request an appointment with Dr. Havranek online or by calling his office at 210-615-8308.